Spine
Dr. Michael Gordon trained at Johns Hopkins University and USC Spinal Cord Injury Center, and has been at the leading edge in spinal surgical technology since he began practice in Newport Beach in 1987. He specializes in a range of spinal surgeries from minimally invasive to complex deformities of the cervical and lumbar spine. Dr. Gordon has extensive experience in complex reconstructive spinal instrumentation surgery of the cervical and lumbar spine as well as disc replacement, adult deformity and degenerative scoliosis.
FAQ - Lumbar Spine Surgery
I’ve just had my MRI of the Lumbar spine - what is a disc herniation and what does it have to do with my sciatic nerve? (The sciatic nerve itself is NOT pinched in disc herniations).
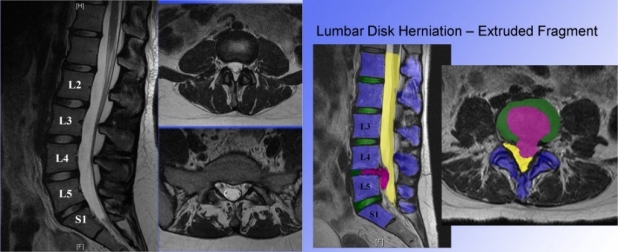
Below on the left is a normal lumbar MRI. There are no disc herniations, pinched nerves, stenosis or arthritic changes at any levels. On the right, there is a large disc herniation causing nerve compression at Lumbar 4-5.
The symptoms of compression of nerve roots in the spine is called sciatica but more formally, lumbar radiculopathy. The sciatic nerve itself is not pinched - it actually is a large nerve that exits the pelvis near the hip. However, pain, numbness, tingling and weakness occurs in the leg due to irritation or compression o f the sciatic nerve at its origin in the spine - hence the word “sciatica”- which describes pain radiation down the leg.
What exactly is a disc herniation, and are there different types of disc herniations? How do they cause nerve pain?
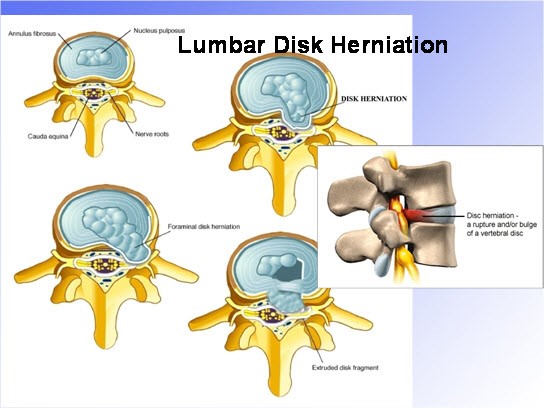
The space between vertebra in the spine is occupied by a complex cartilage and fibrous tissue Disc. Discs provide a cushioning action and allow motion between vertebrae in the spine. The disc itself is made up of two types of cartilage - one fibrous and relatively stiff in the outer ring or annulus- and one of softer cellular material that is more viscous and shock absorbent -the nucleus. The cartilage is not “liquid” but more like very tough gristle.
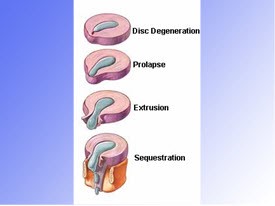
- When discs “herniate” they push through the annular lining of the disc and press on nerves within the spinal canal - hence the word “herniated nucleus pulposus”. Herniations cause nerve pain through a combination of direct nerve compression, and by nerve damage through inflammation. Cells within the disc herniation secrete several substances known to cause direct nerve damage. The larger the disc herniation and the more nerve compression, the more likely there is to be leg pain, numbness and weakness, the signs of nerve damage.
- Disc herniations come in several shapes sizes and locations. They range from small protrusions to large extruded fragments.
- They may be central causing bilateral symptoms, or off to one side (lateral) causing symptoms on only that same side. Mostly disc herniations occur within the spinal canal. Sometimes disc herniations occur outside the spinal canal and are called “extraforamenal” disc herniations.
- Disc herniation sizes can wax and wane with time. Symptoms can come and go as well. Large extruded disc herniations can resorb over time if patients are fortunate. Nerve damage usually improves, but not always, and the longer patients have pain and weakness and numbness, the more likely they are to have permanent nerve damage.
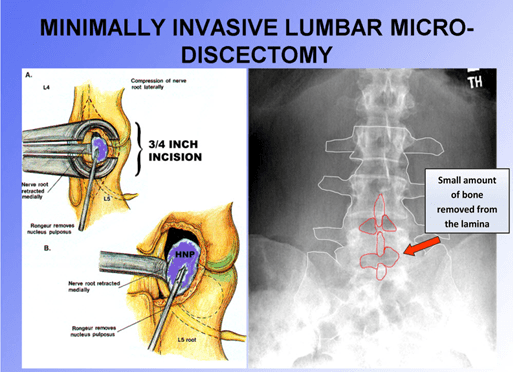
What is a lumbar microdiscectomy?
Microdiscectomy is a minimally-invasive, microscopic-assisted outpatient surgery that is employed to remove herniated discs. Herniated discs cause pressure on nerves in the spine leading to back pain, leg pain, numbness and weakness which are indicative of nerve damage.
What exactly is done during a microdiscectomy surgery?
This is a surgery that is done as an outpatient, but done within the Hoag Hospital Irvine operating room. Specialized equipment is required. It is almost always done under general anesthesia.
A small incision is made in the skin, usually no more than an inch long. It is larger, obviously, in larger and heavier people, and smaller in skinnier people. The muscles of the lower back are carefully moved to the side by especially non-traumatic retractors which prevent muscle injury and limits bleeding. Muscles are not cut during the operation. A small amount of bone - the lamina- is removed from the vertebra to allow access to the spinal canal where the disc is situated. Nerves are then carefully retracted (moved to the side and protected) while the fragments of disc material that press on them are removed. Once nerve compression is relieved, the retractors are removed, the incision is closed usually with one or two sutures, and the skin is closed.
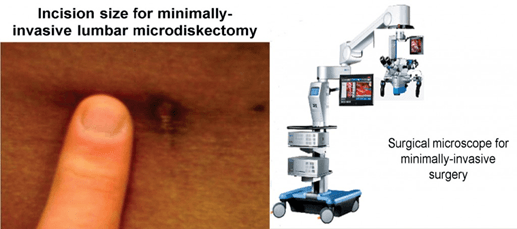
Is this a minimally invasive procedure?
Yes this is a minimally invasive procedure with little or no blood loss, minimal risk, short operating times, and short hospitalizations and short recovery periods
The average incision length is less than one inch. It is often done with the assistance of an operating microscope.
How long does the microdiscectomy operation take?
Most lumbar microdiscectomy procedures last no more than 45 minutes.
Factors that make surgeries take longer include such variables as patient health and “comorbidities” (other diseases such as obesity, heart disease, chronic lung problems or diabetes), patient size, the location of the disc herniation, a history of a prior surgical procedure in the spine, and certain anatomical variants that make the surgery more technically demanding. The RARE microdiscectomy takes more than an hour and a half.
How long will I be in the hospital? Will I go home the same day as an out patient or do I have to spend the night in the hospital?
The entire hospitalization process is usually no more than 5 hours but it is variable. More than 95% of patients go home the same day, feeling improved neurologic function almost immediately. Issues that might make patients spend more time in the hospital include the need for more pain medication, postoperative problems such as nausea or vomiting which occasionally occurs after anesthesia, heart or lung problems that might come up requiring a little more time being monitored in the recovery room or on the hospital floor. Fewer than 5% of patients require an overnight stay.
How long is the recovery period and exactly how is this figured after I have a microdiscectomy?
The word “recovery” means different things to different patients and of course is dependent on many patient-specific issues and pain tolerance. Remember that surgery, however small, is a big stress and as I always remind patients, it is always best to let yourself recover fully with attention to your own well- being.
Let’s consider benchmarks of normal patient recovery after microdiscectomy surgery:
- Out of the hospital and home resting in bed or on a couch - same day.
- Standing and walking - same day.
- Activity restricted to close to home, i.e. 15 minute trips in the car - one to three days postop.
- Return to work - obviously depends on what “work “is...
- Desk jobs requiring mostly sedentary work with little demands for bending stooping and lifting usually are acceptable within 7 days. If the commute is lengthy, such as a 45 minute to 1 hour drive, up to two weeks are usually required before patients are totally comfortable being in the car that long.
- Heavier work involving frequent bending stooping and lifting, or lifting 25 pounds on a regular basis throughout the day requires 3-4 weeks off and a reconditioning exercise program.
- Very heavy work, such as construction, heavy equipment operation, big rig driving, concrete work or pipe fitting (a job where 100 lbs. to 150 lbs. is regularly carried) usually requires 3 months of postoperative recovery.
- We recommend prompt return to sedentary activities on post op day 1. Most daily activities such as preparing a light meal, dressing, bathing, walking around the home, are safe and with the passage of a few days, more activity is tolerated well. A twice daily walk of 15 minutes is an excellent first step in recovery. . A more aggressive exercise program is recommended a week postop. The gym as allowed 3-4 weeks postop and the “straight ahead sports” such as treadmill, elliptical, stair stepper, and pool swimming is encouraged. Light weight training is OK also but we stress no squats, no lunges, and no dead lifts in the first 4-8 weeks.
- Exercise and activities are usually no longer restricted at 10 weeks. We allow golf, tennis and other racquet sports at this time. We caution against lengthy periods of repetitive twisting such as the driving range or tennis-serving drills for 4-6 months. Ocean sports such as surfing, kayaking, paddle boarding are restricted for 10-12 weeks. Very heavy sports activity such as return to football, mountain climbing, marathon running or triathlons, body building as so forth is considered on a case -to -case basis.
What activities can I do, and not do, after a microdiscectomy?
How do I prevent disc herniations from happening?
- Most disc herniations occur randomly throughout populations.
- There is a measurable genetic influence on patients with disc herniations - disc herniation risks cluster in families.
- Many patients blame a specific injury or activity that they feel, if avoided, would have prevented the disc herniation. In the spine surgery literature, there is little evidence for this link between activity and onset of disc herniation.
- Smoking has been associated with an increase in disc degeneration that can lead to increases in disc herniations.
My spine surgeon says I need surgery immediately. What happens if I wait, will there be permanent nerve damage? How will I know if my nerves are permanently damaged?
- If you have severe pain, significant weakness and numbness, and a large disc herniation, DO NOT WAIT.
- There have been many studies on nerve function recovery after surgery, with special attention paid to the time interval between the onset of symptoms and the timing of microdiscectomy surgery. Studies have been done examining groups of patients with disc herniations and leg weakness or numbness who have had surgery soon after the onset of symptoms, or who have waited up to 6 months before having surgery.
- Several nationwide studies show that even with a noticeable degree of pain and weakness, and a large disc herniation, that surgery can be delayed from 3 weeks to even 3 months with no noticeable effect on recovery. This is not to say that, in the presence of a severe foot drop or progressive numbness, that a patient should take a wait-and-see approach.
- The more severe the nerve pain, numbness and weakness, the more likely nerve damage is occurring and the more likely a prompt surgery will allow for full recovery.
- There are no tests that can be done preoperatively that can determine whether a lumbar nerve is permanently damaged. They simply do not currently exist. The only way to determine that permanent damage has occurred to a nerve is to wait for recovery of strength and sensation, and find that patients are not 100% within 1 - 2 years after surgery.
- Therefore, in patients with noticeable weakness, numbness and pain I will suggest prompt surgery to improve the chances of a complete recovery. In patients with minimal findings of numbness and weakness, I will advise a lengthier non-operative approach and can expect recovery without surgery.
Can the disc leak out again in the few months after the surgery? How about later?
- That actually doesn’t happen. Disc material is very tough, like cartilage or gristle on a steak. It doesn’t leak like fluid. It slowly creeps.
- When the disc actually does come out again, it is called either a “recurrent” or “persistent” disc herniation. This is a complicated issue because sometimes, MRI scans done in the immediate postop period see “persistent disc herniations” that are actually only fluid accumulations and cause no problems. MRI scans can be thusly inaccurate in up to 25% of all patients who have NO SYMPTOMS.
- Sometimes, patients have a period of pain and symptom relief for a few months or so and then have symptoms again - I usually wait 4-6 months before getting another MRI because of the “false positive” rates of postop MRI scans that can confuse the issue.
- Reoperation rates within 3 months of surgery are done in rare occasions where the MRI shows a very large “persistent” or “recurrent” disc herniation and patients experience severe symptoms.
What is the reoperation rate after a microdiscectomy?
Reoperation after lumbar microdiscectomy involves several different clinical scenarios with a range of statistical chances of requiring another surgery. The numbers vary according to published studies. Return to the operating room for:
- Washing out the wound due to a superficial infection - 0.5-5%
- Repair of leaking dural puncture not responding to conservative treatment - 0.5%
- Repeat surgery to treat a recurrent disc herniation at the same level - 7-18% at 5 years
- Repeat surgery to treat a recurrent disc herniation at a different level - 5% at 5 years
- Repeat surgery to treat severe disabling back pain requiring fusion - 2% at 5 years
What kinds of complications can occur and how common are they?
- Microdiscectomy surgery is extremely safe, routine, and predictable in the correct hands.
- You will not be maimed, paralyzed, killed nor suffer any major bodily harm. Our main concerns are not the catastrophic outcomes most patients fear, but more mundane problems that occur infrequently. Many patients then ask what exactly are the chances of a problem, and what kind of problem could it be?
- I remind patients that risks from surgery are directly related to the health of the patient, and not surprisingly, the more medical problems one is dealing with such as diabetes, high blood pressure, heart disease, kidney disease, Parkinson’s disease and the like, the higher the risks are.
- I often ask patients to establish other types of risk/benefit scenarios for common human activities so that they can accurately weigh the risk of any surgical procedure. For many of these potential complications, the rates are so small that is has been very difficult to quantify the risk accurately, particularly in the very rare categories and few published articles exist.
To start, let’s consider some other kinds of risk that are associated with everyday life:
- Chance of dying as a result of pregnancy in the USA or Western Europe: 5-10 deaths per 100,000 live births (0.005-0.01%) (Chang 2003, Hill 2001).
-
Risk of death driving on the freeway daily in California per person per
year: 1-3 in 20,000 cars (Cal dept. transportation).
- Risk of drowning in a backyard pool in USA per year : 1 in 100,000
- Risk of being struck by lightning and killed in the USA per year : 1.8 in 10,000,000
ANESTHESIA in HEALTHY PATIENTS:
-
Chance of dying as a result of general anesthesia alone: somewhat less
than 11-16 deaths per 100,000 persons, depending upon general health of
the persons (0.01-0.016%) (Lienhart 2006,
Arbous 2001).
- Chance of dying due to complications resulting from the operation of removing the womb (hysterectomy): 120 to 160 deaths per 100,000 operations (0.12-0.16%) (Bachmann 1990, Loft 1991).
- Chance of dying due to complications resulting from the operation of removing the gallbladder: 150 to 1400 deaths per 100,000 operations, depending upon health and technique of operation (0.15-1.4%) (Feldman 1994, Hannan 1999).
- Chance of dying due to complications resulting from the operation of removing the large bowel for cancer: 800 to 5000 deaths per 100,000 operations, depending upon health and technique of operation (0.8-5.0%) (Nelson-2006).
“Common complications” related to Microdiscectomy surgery:
- Wound infections, all types : 1-6 in 200 (in my practice it is 1 in 200)
- Dural perforations causing CSF leakage requiring repair : 1-10 in 100
- Bleeding requiring return to the operating room : 1-3 in 1,500
- Worsening nerve function after surgery : 2-3 in 200
- Worsening lower back pain after surgery : 5-10 in 200
- Postoperative nausea, vomiting requiring additional hospital day : 1-6 in 200
- Temporary urinary retention requiring catheter insertion 1 in 500
- Temporary worsening of overall pain scores requiring increased meds : 1 in 80
- Permanent worsening of overall pain scores requiring increased meds : 3-15 in 250
- Permanent worsening of lower back pain requiring lumbar fusion in the next 2 years after surgery : 3-15 in 300
- Recurrent disc herniation in the first 3 months after surgery requiring unplanned return to the operating room : 1 in 200
“Rare and Catastrophic” complications from microdiscectomy surgery:
- Death from anesthesia : less than 2 in 100,000
- Paralysis : less than 1 in 250,000
- Loss of bowel or bladder function after surgery : less than 1 in 100,000
What can I expect in the hospital before and after microdiscectomy?
- You will be given medications prior to the surgery to relax you and minimize the likelihood of nausea and vomiting after the surgery.
- You will awaken in the recovery room and be attended one-on-one by a recovery room nurse who will supervise your immediate postop status until you are ready to be discharged.
- From the recovery room, you will either be discharged directly home, or if there is a need, you will be transferred to a room on the orthopedic spine floor for further monitoring.
- Prior to discharge you will be met by several facilitators (nurse case managers and physical therapists) who will insure that you have the appropriate home health needs, appropriate postoperative pain medications, and the appropriate instructions in wound care necessary. You will be given instructions in postoperative exercises and appropriate body mechanics.
When can I go back to work after microdiscectomy?
- This of course depends on the type of work you do. Office based occupations with minimal demands for bending stooping and lifting can usually be resumed within one week. This also depends on how much time is required for commuting and what the office ergonomic environment is.
- Heavy jobs such a maintenance, mechanic or construction work, machinery operators exposed to high vibration and heavy lifting environments require extensive rehabilitation and strengthening prior to return to work.
Is lumbar microdiscectomy a dangerous surgery?
- This is a simple, straightforward, easy, reliable, safe and effective operation.
- I have personally performed over 2,000 discectomy surgeries and I can say without reservation, this is one of the safest spinal surgeries I perform with minimal risk and predictable outcomes.
- Safety arises because of my strict adherence to appropriate perioperative monitoring, highest professionalism in my anesthesia team and intraoperative nursing, and careful attention to detail in the operating room. I am meticulous regarding appropriate diagnostics and patient selection to insure good outcomes
I hear all my relatives and friends say never have any back surgery, and that paralysis is a risk.
- With no disrespect to your friends and family, if they have a lengthy experience with spine surgery you should listen to them. Otherwise be cautious about their advice.
- Spine surgery, particularly microdiscectomy, is extremely safe particularly if your surgeon does ONLY spine surgery. Nationally, there is less than 1 in 250,000 chance of a severe neurologic catastrophe and it usually has very little to do with the actual surgery, but more often to issues with underlying defects of circulation within the nerves themselves.
- Spine surgery can be life and limb saving if done appropriately and at the correct time. Patients should not allow themselves, because of their fear of surgery, to deteriorate to the point where we cannot help them. We understand that spine surgery is more complex than many other types of surgeries, but can assure patients that we can explain all the risks and benefits associated with spinal procedures.
- Over the last 20 years, there has been a remarkable advancement in the accuracy of diagnostics and the lessening of the stresses of surgery that has enabled much better outcomes and much safer surgeries. Spine surgery has suffered from a very bad reputation among patients and family members. This stems from admittedly poor diagnostic information and rudimentary understanding of the nature of spinal problems and procedures that came from the “early days” of spine surgery in the 1950’s and 1960’s.
I’ve been told there is a “laser alternative” and have seen many advertisements on TV and on the internet. This sounds like a lot of hype, but I’ve heard it so often I’m not sure.
- It is safe to say that lasers have no place in my practice of spine surgery, and very few surgeons in the USA find any value in the laser used during spinal surgery. Incidentally, lasers cannot cut bone easily, but they DO cut nerves easily.
- The following hospitals DO NOT have a laser for spine surgery (you can imagine if it was a useful tool it would be widely used):
- Hoag Hospital, Mission Hospital, Saddleback Hospital, Long Beach Memorial
- UCLA, USC, UC Santa Barbara, UC San Diego, UC San Francisco
- Scripps, Mayo Clinic, Johns Hopkins Hospital
- There is no “truth-in-advertising” with regard to medicine. Any practitioner can state anything in print and make even the most outrageous claims about “remarkable new advances” and “miraculous recoveries” without having to provide any proof. Unfortunately the “LASER Institute” and other similar companies fall into this hype categorization. Statements such as, “no one else in the country has this technology,” or, ”we are the only ones who have perfected this procedure and no one else can do it” should be recognized for what they are: unsubstantiated.
- As a general rule in medicine, the larger and splashier the advertisement, and the more remarkable the claims, the less likely the information is true. IF IT SOUNDS TOO GOOD TO BE TRUE!!!!, AND MOST INSURANCES ARE ACCEPTED!!!, AND YOU CAN COME IN FOR A FREE EVALUATION!!!!, AND WE ARE THE ONLY ONES WITH A SPECIAL PATENTED APPROACH, AND WE HAVE LOTS OF PATIENT TESTIMONIALS!!!!, AND IT’S COMPLETELY BLOODLESS SURGERY!!! THEN YOU SHOULD BE VERY SUSPICIOUS AND VERY AFRAID.
I’ve been told there is an arthroscopic alternative.
I’ve been told specialized traction from my chiropractor will help reduce the size of my disc herniation.
- There is no evidence traction of any kind; even “the spinal decompression variety” has any effect on the size of a disc herniation, more than the passage of time.
- There are no published articles in any reliable journals of spine surgery (Spine, Journal of Neurosurgery, Clinical Orthopedics, NASS Spine Journal, European Spine Journal, Spinal Disorders, Journal of Bone and Joint Surgery) that demonstrate effectiveness of traction beyond that of any other physical therapy modality.
- Chiropractic manipulations, particularly vigorous, of the lumbar spine in the presence of a large disc herniation, and with associated neurologic findings such as numbness tingling or weakness, should be avoided.
What activities do I have to avoid in order to prevent a recurrence?
- Avoidance of heavy or repetitive bending stooping and lifting tasks can help to minimize the reoccurrence of a lumbar disc herniation.
- Interestingly, after many decades of study, the only clear predictors of disc recurrence are the initial size of the disc herniation at surgery, and the amount of disc material removed at surgery.
- In other words, very large disc herniations recur more often than small ones. Removing more disc material at surgery decreases the recurrence rate at the expense of slightly increasing the amount of postoperative low back pain.
When can I have sex again?
- Let the wound heal first. Keep the wound off the bed. Use some common sense (sometimes hard in matters of the heart, but really...)
What kind of anesthesia is used?
- General anesthesia is the preferred method of anesthesia at Hoag Orthopedic Institute for outpatient spinal surgery. It is safe and well-tolerated with a minimum of side effects.
What sorts of things should I do in preparation for surgery?
- Quit smoking if you do smoke.
- Minimize the use of narcotic medications.
- Minimize alcohol use.
- Make sure your diabetes or blood pressure or heart medications are up to date.
- If required, get your preop medical evaluation as soon as possible.
- Get informed about the procedure.
- Plan your postoperative regimen of appropriate diet, exercise and ergonomic modifications at home and work.
How many of these microdiscectomies have you done?
- I’ve been in practice doing nothing but spine surgery since 1987. I average 250 spine procedures per year or more. It is common for me to do between 100 and 150 lumbar discectomies a year. I estimate I’ve done more than 2,000 microdiscectomies.
I want a second opinion.
- Our favorite patients are those who are comfortable with their physicians, understand the nature of the surgery being recommended, and who feel their questions have been adequately answered. We understand that when faced with a spine surgery many patients want other opinions and we encourage this practice. We can provide the names of other spine professionals in the area who we believe offer the same level of expertise that we can offer.
Do I need a fusion with a discectomy? This is a recurrent disc herniation I now have after the first surgery. What is different about the approach towards surgery in this case?
- More than 90% of spine surgeons (including me) polled recently by the North American Spine Society report that they “never” perform a fusion at the time of a microdiscectomy for disc herniation.
- If there is a recurrent disc herniation requiring surgery, the vast majority of spine surgeons will perform a repeat microdiscectomy at the time of a first recurrence of a disc herniation. Most will fuse a vertebral segment if the disc herniation recurs a second time. In other words, the first two disc herniations are treated with microdiscectomy, the third with a fusion. On occasion these rules will be bent depending on the type of findings and symptoms - back vs leg pain, degree of degeneration and/or instability seen on MRI.
What’s the difference between a neurosurgeon and an orthopedic surgeon in the field of spine surgery?
- The short answer is NOT MUCH if the surgeons are trained in SPINE. Orthopedics and Neurosurgery share responsibilities in spine surgery, although most spine surgery in the United States is done by Orthopedic Surgeons with subspecialty Fellowship Training in Spine Surgery. We recommend that spine surgery be performed by surgeons whose practice is exclusively devoted to spine surgery. This is a trend that has been reinforced in the last fifteen years in the USA because, given the complexity of spinal surgery even as compared to brain surgery, better outcomes are seen with surgeons whose only focus is spine surgery. We recommend that ALL spine surgery be performed by surgeons who have passed the American Board of Orthopedic Surgery specialty examination in Spine Surgery (or the equivalent in Neurosurgery). Whether your surgeon began his or her training as an Orthopedic Surgeon or a Neurosurgeon, the important issue is the additional training requirements to be subspecialty-trained in spine surgery. Generally speaking, the notion that “a Neurosurgeon is somehow better acquainted with nerves” is an antiquated idea, and with no disrespect to my neurosurgical colleagues.